
When Memories Fade, Hold onto the Moments
The human brain is the most complicated structure known in the cosmos. This spongy mass of fat and protein known as the brain is made up of two types of cells termed glia and neurons, both of which number in the billions. Neurons are distinguished by their axons and dendrites, which are branch-like projections that gather and send electrochemical impulses. This complicated network of cells, when combined, gives rise to every facet of our shared humanity. Without the brain, we couldn’t breathe, play, love, or remember. Humans value thoughts, feelings, consciousness, and cognitive abilities, all of which are tied to the human brain.
When a person loses track of time, forgets day-to-day critical chores, and is unable to remember the most familiar faces, it is considered a problem, and this is most common in the elderly community. This is referred by the doctors as Alzheimer’s disease or Dementia. This disorder affects millions of individuals and becomes more frequent as people age (approximately one-third of all persons aged 85 and older may have some type of dementia), yet it is not a normal part of the aging process. Many people live well into their 90s and beyond without showing any signs of dementia. There are numerous types of dementia, the most common of which is Alzheimer’s disease.
The most frequent form of dementia is Alzheimer’s disease, which is characterized by a steady increase of short-term memory loss, disorientation, and mood changes. It is the sixth biggest cause of death in the United States, and its prevalence is increasing. Alzheimer’s disease or another kind of dementia affects around 50 million individuals worldwide. While there are a few medications available to help with Alzheimer’s symptoms, there is no cure. Researchers all across the world are working on cures that could one day put a stop to the disease’s devastation.
If you’re looking for information on Alzheimer’s and the type of care an Alzheimer’s patient requires, you’ve come to the right place. Keep reading to find out what Sirwiss-affiliated care provider service experts have to say about Alzheimer’s.
What Is Alzheimer’s Disease?

Alzheimer’s disease is a brain disorder that gradually deteriorates memory and thinking abilities, as well as the ability to do basic tasks. Symptoms of Alzheimer’s disease usually show later in life in the majority of people. Experts estimate that more than 6 million, the majority of whom are 65 or older, may have Alzheimer’s disease. Alzheimer’s disease is the seventh largest cause of death in the United States and the primary cause of dementia in older persons.
The causes of dementia might vary based on the type of brain abnormalities that are occurring. Other types of dementia include Lewy body dementia, frontotemporal diseases, and vascular dementia. It is typical for people to have mixed dementia, which is a combination of two or more kinds of dementia. Some patients, for example, have Alzheimer’s disease as well as vascular dementia.
How Does Alzheimer’s Disease Affect the Brain?
Scientists are still working to understand the complicated brain alterations that occur in Alzheimer’s disease. Brain changes can begin a decade or more before symptoms arise. Toxic alterations occur in the brain during this early stage of Alzheimer’s, including aberrant protein buildups that generate amyloid plaques and tau tangles. Consequently, healthy neurons stop working, lose connections to neighboring neurons, and eventually die. Many more complicated brain alterations are known to contribute to Alzheimer’s disease.
The damage appears to begin in the hippocampus and the entorhinal cortex, two areas of the brain important for memory formation. As more neurons die, more areas of the brain become impacted and begin to shrink. Damage is pervasive at the end stage of Alzheimer’s, and brain tissue has shrunk significantly.
Signs and Symptoms of Alzheimer’s Disease
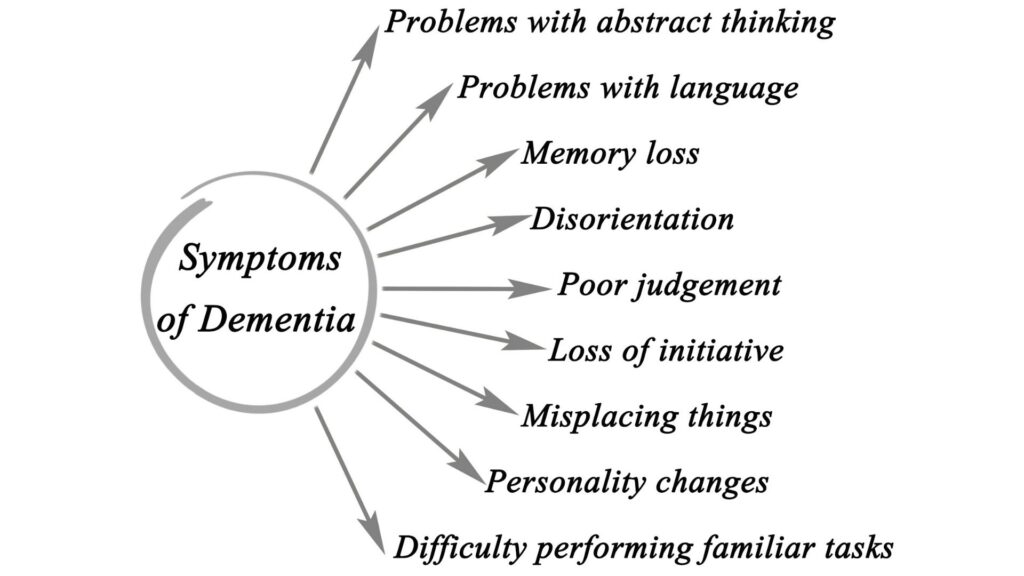
Memory issues are frequently one of the earliest indicators of Alzheimer’s-related cognitive decline. Mild cognitive impairment (MCI) is a condition that affects some persons who have memory impairments. People with MCI have more memory impairments than is typical for their age, but their symptoms do not interfere with their daily life. MCI has also been associated to difficulty with movement and the sense of smell. Older adults with MCI are more likely to develop Alzheimer’s disease, but not all of them do. Some people may even regain normal cognition.
The initial signs of Alzheimer’s disease differ from person to person. Nonmemory components of cognition, such as word searching, vision/spatial difficulties, and impaired thinking or judgment, may signify the very early stages of the disease for many people. Biomarkers (biological indicators of disease detected in brain imaging, cerebrospinal fluid, and blood) are being studied by researchers to detect early changes in the brains of persons with MCI and cognitively normal people who may be at higher risk for Alzheimer’s. More study is needed before these techniques may be used widely and consistently to identify Alzheimer’s disease in the office of a health care provider.
Stages of Alzheimer’s
1. Mild Alzheimer’s
Memory loss and other cognitive impairments develop as Alzheimer’s disease progresses. Wandering and getting lost are examples of problems, as are difficulties handling money and paying bills, repeating inquiries, taking longer to do typical everyday duties, and changes in attitude and conduct. People are frequently diagnosed at this point.
2. Moderate Alzheimer’s
During this stage, injury occurs in regions of the brain that regulate language, reasoning, conscious thought, and sensory processing, such as the ability to accurately detect sounds and odors. Memory loss and confusion worsen, and individuals have difficulty recognizing family and acquaintances. They may be unable to acquire new information, perform multistep tasks such as dressing, or adapt to novel situations. In addition, individuals at this stage may exhibit hallucinations, delusions, and paranoia, as well as impulsive behavior.
3. Severe Alzheimer’s
Ultimately, plaques and tangles spread throughout the brain, and brain tissue shrinks significantly. People with severe Alzheimer’s cannot communicate and are completely dependent on others for their care. Near the end of life, the person may be in bed most or all of the time as the body shuts down.
Causes of Alzheimer’s Disease

Scientists have made tremendous strides in comprehending Alzheimer’s disease in recent years, and the momentum continues to grow. Still, scientists do not completely comprehend the causes of Alzheimer’s disease in the majority of patients. Age-related alterations in the brain, along with genetic, environmental, and lifestyle factors, are likely contributors. The relevance of any one of these factors in increasing or decreasing the risk of Alzheimer’s disease may vary from individual to individual.
Genetics and Alzheimer’s Disease
In most cases, there is no single genetic cause for Alzheimer’s. Rather, it is likely influenced by a combination of multiple genes, lifestyle, and environmental factors. Genetic variations can either increase or decrease a person’s risk of developing a disease.
Currently, scientists are aware of over seventy genetic regions associated with Alzheimer’s. Only three genetic variants associated with Alzheimer’s disease are known to be disease-causing. When a person inherits a variant of one of these genes — APP, PSEN1, or PSEN2 — it is likely that they will develop Alzheimer’s before age 65, and sometimes much earlier. Individuals with Down syndrome have an increased risk of developing Alzheimer’s disease earlier in life.
Health, Environmental, and Lifestyle Factors
Multiple factors outside of genetics may play a role in the onset and progression of Alzheimer’s disease, according to research. For instance, there is a great deal of interest in the connection between cognitive decline and vascular conditions, such as heart disease, stroke, and high blood pressure, as well as metabolic conditions, such as diabetes and obesity. Ongoing research will help us determine whether and how reducing risk factors for these diseases can also reduce the risk of Alzheimer’s.
A nutritious diet, physical activity, social interaction, and mentally stimulating pursuits have all been linked to helping people maintain their health as they get older. These elements may also reduce the risk of cognitive decline and Alzheimer’s. Clinical trials are being conducted to evaluate a number of these hypotheses.
Diagnosing Alzheimer’s
Doctors use a variety of techniques and diagnostic instruments to determine whether a patient with memory problems has Alzheimer’s.
- Ask the person and a family member or friend questions about overall health, use of prescription and over-the-counter medicines, diet, past medical problems, ability to carry out daily activities, and changes in behavior and personality.
- Conduct tests of memory, problem solving, attention, counting, and language.
- Order blood, urine, and other standard medical tests to help identify other possible causes of the problem.
- Administer tests to determine if depression or another mental health condition is causing or contributing to a person’s symptoms.
- Collect cerebrospinal fluid via a spinal tap or order blood tests to measure the levels of proteins associated with Alzheimer’s and related dementias.
- Perform brain scans, such as CT, MRI, or PET (positron emission tomography), to support an Alzheimer’s diagnosis or to rule out other possible causes for symptoms.
These tests may be administered multiple times in order to provide physicians with information on how a patient’s memory and other cognitive functions change over time.
People with memory and thinking issues should consult a physician to determine whether their symptoms are due to Alzheimer’s disease or another condition, such as a stroke, tumor, Parkinson’s disease, sleep disturbances, medication side effects, an infection, or another form of dementia. Some of these conditions may be reversible and/or treatable.
How is Alzheimer’s Treated?
Due to the complexity of Alzheimer’s, it is unlikely that a single drug or other intervention will be able to successfully treat the disease in all patients. In ongoing clinical trials, researchers are devising and evaluating multiple potential treatment interventions.
While there is presently no cure for Alzheimer’s, new drugs are being developed to treat the disease’s progression by addressing its underlying causes. There are also medications that may temporarily enhance or stabilize memory and cognitive abilities in some individuals, as well as aid in the management of specific symptoms and behavioral issues.
In addition, Alzheimer’s patients may suffer from insomnia, melancholy, anxiety, agitation, and other behavioral and psychological symptoms. Scientists continue to investigate the causes of these symptoms and are investigating new medications and non-drug strategies for treating them.
Caregivers and Families of People with Alzheimer’s

For many families, providing for a person with dementia is not the sole responsibility of a single individual, but rather a shared responsibility among multiple individuals. Sometimes a caregiver or custodian resides with or nearby the individual. Regardless of the type of caregiver you are, caring for another person can at times be overwhelming. These guidelines and suggestions may be useful for routine care and chores.
Everyday Care
Early on in Alzheimer’s disease and other dementias, individuals experience changes in thinking, remembering, and reasoning that have a significant impact on daily life and activities. Eventually, individuals with these illnesses will require more assistance with simple, daily duties. This may include hygiene, bathing, and dressing. It can be upsetting for a person to require assistance with such intimate tasks.
Here are a few tips to keep in mind as the disease progresses and as it first appears:
- Try to keep a routine, such as bathing, dressing, and eating at the same time each day.
- Help the person write down to-do lists, appointments, and events in a notebook or calendar.
- Plan activities that the person enjoys and try to do them at the same time each day.
- Consider a system or reminders for helping those who must take medications regularly.
- When dressing or bathing, allow the person to do as much as possible.
- Buy loose-fitting, comfortable, easy-to-use clothing, such as clothes with elastic waistbands, fabric fasteners, or large zipper pulls instead of shoelaces, buttons, or buckles.
- Use a sturdy shower chair to support a person who is unsteady and to prevent falls. You can buy shower chairs at drug stores and medical supply stores.
- Be gentle and respectful. Tell the person what you are going to do, step by step while you help them bathe or get dressed.
- Serve meals in a consistent, familiar place and give the person enough time to eat.
Changes in Communication and Behavior
Because they have difficulty remembering things, Alzheimer’s and related dementia can make communication difficult. In addition, they can become agitated, anxious, and even furious. In some forms of dementia, language abilities are impaired to the extent that patients have difficulty finding the appropriate words or speaking. You may feel frustrated or impatient, but it is essential to realize that the change in communication skills is due to a disease.
To facilitate communication, you can:
- Reassure the person. Speak calmly. Listen to his or her concerns and frustrations. Try to show that you understand if the person is angry or fearful.
- Allow the person to keep as much control over8ygy his or her life as possible.
- Respect the person’s personal space.
- Build quiet times into the day, along with activities.
- Keep well-loved objects and photographs around the house to help the person feel more secure.
- Remind the person who you are if he or she doesn’t remember, but try not to say, “Don’t you remember?”
- Encourage a two-way conversation for as long as possible.
- Try distracting the person with an activity, such as a familiar book or photo album, if you are having trouble communicating with words.
Healthy and Active Lifestyle for People with Alzheimer’s
Eating well and staying active are beneficial for everyone, but they are especially essential for those with Alzheimer’s disease and other dementias. As the disease progresses, it may become increasingly difficult for the individual to consume nutritious foods and maintain an active lifestyle.
Here are some helpful suggestions:
- Consider different activities the person can do to stay active, such as household chores, cooking and baking, exercise, and gardening. Match the activity to what the person can do.
- Help get an activity started or join in to make the activity more fun. People with dementia may lack interest or initiative and can have trouble starting activities. But, if others do the planning, they may join in.
- Add music to exercises or activities if it helps motivate the person. Dance to the music if possible.
- Be realistic about how much activity can be done at one time. Several short “mini workouts” may be best.
- Take a walk together each day. Exercise is good for caregivers, too!
- Buy a variety of healthy foods, but consider food that is easy to prepare, such as premade salads and single portions.
- Give the person choices about what to eat, for example, “Would you like yogurt or cottage cheese?”
Home Safety
As a caregiver or family member of an individual with Alzheimer’s disease or a related dementia, you can take measures to make the home a safer environment. By removing hazards and adding safety features to the residence, the individual can move around more independently and safely.
Try the following:
- If you have stairs, make sure there is at least one handrail. Put carpet or safety grip strips on stairs or mark the edges of steps with brightly colored tape so they are more visible.
- Insert safety plugs into unused electrical outlets and consider safety latches on cabinet doors.
- Clear away unused items and remove small rugs, electrical cords, and other items the person may trip over.
- Make sure all rooms and outdoor areas the person visits have good lighting.
- Remove curtains and rugs with busy patterns that may confuse the person.
- Remove or lock up cleaning and household products, such as paint thinner and matches.
Being a caregiver can be both incredibly rewarding and overwhelming. It requires time and effort to care for a person with Alzheimer’s or a related dementia. It can be isolating and aggravating. You may even experience anger, which could be an indication that you are attempting to take on too much. It is essential to schedule time for self-care. It is always prudent to allow a professional caregiver to assist your loved one who suffers from this debilitating illness.